Six months after WHO declared COVID-19 a global pandemic, Power Diary launched a research project to understand how the pandemic has impacted allied health practices. We received 478 responses to our detailed survey from allied practices predominantly located in the UK, Australia, New Zealand and the USA. The findings were enlightening and many things stood out as significant and somewhat surprising.
Our key insights on the Coronavirus impact on allied health practices are as follows:
- The demand for some professions has increased significantly. Most notably, many psychologists & mental health professionals, speech pathologists, and occupational therapists have experienced an increase in demand.
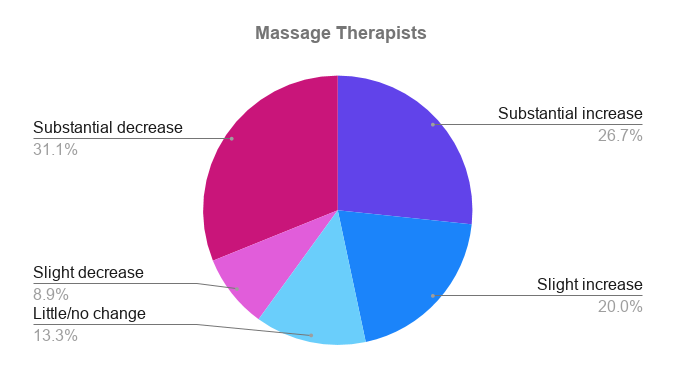
- The hardest-hit allied health professions have been physiotherapists, massage therapists, naturopaths and other alternative health practices.
- Podiatrists were polarised with slightly more than half experiencing increased demand, and the other half experiencing a lower demand.
- Concerningly, an overwhelming 77% of respondents reported an increase in stress levels with 27% reporting this to be a substantial increase.
- 3 out of 4 allied health practices are now using Telehealth as a service delivery method, with the vast majority (81%) also intending to continue using Telehealth in some form once the pandemic passes.
- Most allied health practices have implemented many new protocols to address the risks associated with Coronavirus. These include; measures to inform clients and conduct health checks before appointments, physical protection aids, new cleaning protocols, measures to reduce contact, social distancing protocols, and new policies.
- As a result of additional cleaning protocols, some allied health practices now have significantly less time to see clients, and while most have made modest investments in new infrastructure and supplies, some have spent thousands.
- The biggest challenges for health practices as a result of the pandemic were found to be; financial pressures, client stress, adopting new technologies, managing increased demand, uncertainty around government policies, team & self-management, managing increased communication, personal stress levels, wearing masks, cleaning protocols, and keeping informed of changes.
- There were also some surprising positive effects which have come from the pandemic. These include a heightened focus on health, benefits associated with moving online, fewer sick clients, increased attention to hygiene, a quieter pace (both at home and in practices), community camaraderie, time to focus on improvements, and for some, increased business opportunities.
To drill into the findings in more detail, let’s go through the different result areas…
Changes in Customer Demand Since the COVID Pandemic
We were curious to know how customer demand has been impacted since the start of the pandemic. The results varied dramatically by profession, and even within professions, we saw a large variation. Here is a summary, broken down by profession:
Changes in the Personal Stress Levels of Allied Health Professionals
With all the demands on health practitioners, we were curious to know if the COVID pandemic had impacted on stress levels. We were shocked to find that an overwhelming 77% of respondents reported an increase in stress levels with 27% reporting this to be a substantial increase.

The specific question we asked here was “Compared with pre-Coronavirus, what effect has the pandemic had on your personal stress levels in relation to seeing your clients?”. The fact that 77% of practitioners are reporting increased stress about seeing clients is very significant. Of course, this could be due to many factors including increased (or decreased) demand, the protocols involved with seeing clients, or the state of mind of the clients themselves.
The impact of increased stress should not be underestimated though and measures to mitigate this should be regarded as high priority.
Client Hesitation and Fear around In-Person Sessions
Even though most private practices have been able to continue operating for the majority of the time, we were curious to know how clients are coping and how their mindset has changed. Despite this being a projection, we asked practitioners to state their thoughts on how the Coronavirus has impacted on client hesitation and fears when it comes to in-person sessions.
49% reported that some clients had slight hesitation or fear, 24% said there was significant fear or hesitation in some clients, and 7% said there was significant fear or hesitation in a large proportion of clients.

Implementation of Telehealth Since the Coronavirus Pandemic
Although some allied health practices already offered their services via Telehealth, many have introduced Telehealth since the COVID Pandemic began. In fact, 75% of the practitioners that completed our survey now use Telehealth to some extent.

Of the clinics using Telehealth, 54% of them say that Telehealth sessions account for half or more of their appointments, and 27% are using Telehealth for “Almost All” of their sessions. And interestingly, more than 53% state they will ‘definitely’ continue using Telehealth once the pandemic passes and another 27% say they will ‘probably’ continue using Telehealth (and only 7% say they will ‘probably not’ continue with it).
Uptake of Telehealth by Profession
Of course, the use of Telehealth varies by the type of allied health service. Here is a breakdown of the professions using Telehealth:
- Physiotherapists – 75%
- Psychologists & Mental Health Professionals – 95%
- Massage Therapists – 6%
- Speech Pathologists – 96%
- Podiatrists – 0%
- Occupational Therapists – 100%
- Chiropractors & Osteopaths – 11%
- Nutritionists & Dieticians – 71%
- Naturopaths & Other Alternative Health Practices – 40%

Reasons to Continue Using Telehealth
When we dug into the reasons behind why these health practices intend to continue using Telehealth, the responses tended to fall into the following categories:
- Flexibility for clients that find it difficult to access a clinic
Some of the comments from respondents included:- “I will be continuing as it is a very convenient way for clients to receive therapy. Particularly in relation to no travel time for people who work, mothers unable to find babysitters, more convenient for disabled or chronically ill, couples can connect from different locations, and generally speaking it is just far more convenient in the busy world we live in.”
- Another said, “Telehealth has proven to have the same positive impact and benefits as in-person therapy. It is more flexible around client schedules and commitments and clients are able to access their therapy from any location.”
- And another, “We will be, as we have found a need amongst our clients who find Telehealth really helpful. Whether it be a client who doesn’t have a car and has to travel a long distance, a parent with a sick child who cannot leave the house, or someone who uses their long lunch break to have an appointment in a private office.”
- Ability to service clients from a wider geographic area
Some comments from practitioners include:- “Provides a flexible approach to service provision and extends the reach of our practice.”
- “I have clients move away but they can still see me. Opens up more opportunities.”
- And another perspective was; “I work within a very niche client area – Telehealth has allowed me to offer services to those that fit my niche but do not live locally or who cannot find an alternative provider from this niche close to them.”
- “Telehealth has been a great way to support clients who have moved to other states. Normally you would lose these clients.”
- Ability to service clients with health issues
This includes situations where clients may be contagious and should not come into the clinic, as well as clients with chronic issues or difficulties travelling. Some comments from respondents included:- “We use it when clients are sick – to reduce the risk of infection for practitioners.”
- “Convenience for clients that may have a sniffle but can still attend.”
- “Implementing Telehealth has been a saviour for many of our most anxious clients during the pandemic. We will continue to use this platform for our clients in the future for any unwell, anxious clients who are having trouble commuting or simply are unable to make it to the clinic. Our clients and psychologists have adapted really well to Telehealth. It has saved many clients from cancelling their appointments knowing we have Telehealth in place.”
- A fall-back option or a supplement to face-to-face appointments
A few respondents mentioned that they would keep Telehealth in place purely as a fall-back option, in case anything like the COVID Pandemic ever happened again.- Others mentioned that they find it helpful to have a balance of face-to-face and Telehealth appointments.
- “It’s going to be a great supplement to help people with their home programmes. It’s very time efficient and more profitable than seeing patients face-to-face on home visits.”
- Some practices intend to use Telehealth in addition to face-to-face sessions, e.g. “for reviewing goals and checking in with clients and their support workers”.
- Client preference for Telehealth
And many cited that their clients actually just prefer Telehealth sessions:- “A greater percentage of clients prefer this method of counselling.”
- “Some clients feel safer in their own home due to trauma histories and I’ve found it can speed up progress.”
- Practitioner preference for Telehealth
- Some also stated that they “like working from home” or feel that Telehealth sessions are “more focused and effective”.
- Another mentioned, “Telehealth has been the only real positive to come out of the pandemic. For existing clients, it enables much more regular attendance of sessions and therefore better outcomes.”
- Flexibility for managing practitioners
Many also highlighted that Telehealth offers a lot of benefits for practice management in terms of how practitioners can be scheduled. Some comments included:- “We can now spread the load over clinicians in multiple locations”
- “We have now brought on remote psychs to help with managing demand for appointments”
However, many respondents also stated that their continuation of Telehealth will depend on whether these treatments continue to be covered by the relevant national health systems in their country. This is a big concern for many.
Reasons Some Practices have Not Implemented Telehealth
Of the practices not using Telehealth, the reasons behind their decision tended to fall into the following categories:
- Not suitable for their profession
As seen in the industry breakdown earlier, Telehealth is more suited to some professions than others. It is not suitable for hands-on, manual therapies, notably massage, podiatry, acupuncture, chiropractic work, as well as some physiotherapy. Or as one respondent put it “Telehealth hasn’t got human hands!”
- Have not had the need
In some cases, practitioners have not been especially affected by the COVID Pandemic, so Telehealth has not been a priority.
- Not suitable for their client profile
Others stated that the type of clients they see make Telehealth more challenging. For example, one respondent stated that Telehealth is “Sometimes difficult with the attention span of the children.” Others cited difficulties with older patients or patients with disabilities.
- Client reluctance
There were some respondents who cited client reluctance or preference for face-to-face sessions as the reason they hadn’t implemented Telehealth. Others simply said they had not had any demand from clients.
- Poor internet connectivity
A small minority cited weak internet as the reason they had not been able to use Telehealth.
New Protocols in Allied Health Practices to Address Coronavirus Risks
Almost all health practices have put in place new measures specifically to address the risks associated with COVID infection. The most common amongst these include:
- Measures to educate clients and conduct health checks before appointments:
- Online questionnaires to ask clients if they have symptoms
- Telephone screening
- Temperature checks on arrival
- Signage to educate and remind patients of protocols
- Provision of instructions, FAQ’s and guidelines for Telehealth
- Sending COVID symptom reminders in SMS reminder messages
- Physical protection
- Mandatory masks for practitioners and (in most cases) patients
- Hand sanitiser stations
- Perspex screens
- Perspex visors for practitioners
- Improved ventilation
- New cleaning protocols
- This was mentioned by almost all respondents, and for many, has been a significant adjustment (see next section)
- Measures to reduce contact
- Offering Telehealth sessions (exclusively or by default)
- Online forms – especially intake and consent forms
- Online payments (not allowing cash payments)
- Eliminating tea/coffee facilities and snacks for clients
- Removing magazines from waiting rooms
- Reduced toys (or rotating and cleaning more often), or asking clients to bring their own toys
- Removing other items (e.g. fidget toys, weighted blankets)
- No handshakes
- Paper towels in the kitchen (in place of cloth towels)
- Disposable cups for water
- Pedal bins
- Reduced client access to toilets/bathrooms
- Social distancing protocols
- Spaced furniture in waiting rooms/reduced furniture
- Limits on the number of people in waiting rooms – many require clients to wait in their cars
- Social distancing – particularly relevant for waiting rooms and reception desks
- Signage/lines on the floor for walkways, separate entry/exit passages
- Gaps between appointments (to clean and also minimise contact between patients)
- Restrictions on bringing extra people to appointments (e.g. no siblings of children being treated, one parent only)
- New policies
- Not allowing patients to attend if they have any symptoms
- No cancellation fees for people being unwell (to encourage them to disclose this)
- Contact tracing
- “Work bubbles” for rostering staff on together with the same group each time
Impact of Additional Cleaning Measures
Almost 89% of respondents reported that they have implemented additional cleaning measures, specifically to cope with the threat of Coronavirus. Most that answered ‘No’ to this question stated that they already had sufficient measures in place.

The most frequent descriptions of the changes put in place for cleaning measures included:
- Increased frequency of cleaning, most commonly after every client
- Increased attention to cleaning anything that has been touched (door handles, handrails, chairs, computers, pens, EFTPOS terminals, etc)
- Increased use of disinfectant sprays
- Airing of rooms between appointments
- Practitioners changing gowns between appointments
- Increased usage (frequency or length) of professional cleaners
Some practices felt that these increased cleaning protocols have reduced their ability to see clients. However, only 4% reported that their availability was drastically reduced and 17% reported that their availability was moderately reduced.

New Infrastructure put in Place in Allied Health Practices
The most common infrastructure changes have been to remove items (e.g. some chairs, soft toys, etc). But many allied health practices have also needed to invest in new infrastructure in order to address the Coronavirus risks and continue operating their practices.
The most common investments are:
- Perspex screens for reception areas
- Plastic covers on seats (to allow easier cleaning), some also changed to more cleanable furniture
- Replaced soft toys with wipeable toys
- New signage
- New laptops and headsets (for practitioners conducting Telehealth sessions)
- QR code check-in/electronic door access/video doorbell
- Thermometers
- Air ventilators/cleaners
- UV lights/light wands
About one third of practices have spent between $200/£200 on new infrastructure, and another third of practices state that they have spent > $1000/£1000 on new infrastructure. However, there are several health practices who reported spending over $15,000/£15,000 on COVID-related infrastructure!
Additional Costs Related to COVID Precautions
Of course, health practices are also bearing the costs of the extra materials needed to mitigate COVID risks as well. Items commonly cited were:
- Hand sanitiser
- Disposable face masks
- Face shields
- Surgical gloves
- Wipes
- Paper towels
- Disinfectant
These items are generally not too costly and most reported spending somewhere between $10-$150/£10-£150 per week.
However, most practitioners stated that the biggest ongoing cost is actually their time and that of their team, plus, in some cases, the reduced ability to see clients.
Biggest Challenges for Health Practices During the Pandemic
Clearly, the Covid Pandemic is affecting us all differently, but when it comes to Allied Health Practices, the biggest challenges they are facing appear to be as follows:
- Financial pressures
- Client stress
- Adopting new technologies
- Managing increased demand
- Uncertainty around government policies
- Team & self-management
- Managing increased communication
- Personal stress levels
- Wearing masks
- Cleaning protocols
- Keeping informed of changes
When we dig into these areas to understand exactly how allied health practitioners are being affected, it’s easier to get a real feeling for the types of situations they are experiencing.
- Financial pressures (or being forced to close)
For many, the closures have led to a severe drop in client numbers and financial issues. Some state they are unsure as to whether they will be able to open up again. For others, they are still able to operate but either in a reduced capacity, or with reduced customers. As one practitioner put it, the difficulties arise from having “increased costs, but reduced income.”
In this regard, many practice owners mentioned that they were actively negotiating reduced rental arrangements and/or accessing government supplements as a way to minimise the financial impacts on their business.
- Client stress
Many practitioners noted client stress as one of the top challenges. They stated that “patient anxiety levels have increased dramatically”. Other comments included:- The difficulties with “watching the devastating effect it is having on my patients.”
- In addition, client stress is causing some of them to avoid treatment with one practitioner saying; “Many of our clients are too scared to return.”
- “Clients’ anxiety is heightened, leading to verbal abuse on the phone to the Admin staff. Everyone wants an appointment NOW and they become distressed when there is no availability.”
- Overall, there is “increased stress for many clients, e.g. fears relating to the pandemic, social isolation, and reduced opportunities to connect with others, and immense loneliness”.
- Adopting new technologies
For many, the challenge of introducing new technologies and the associated processes proved difficult. (Although many also report this as one of the eventual positives of the situation as well.) Some practitioners stated their biggest challenges as follows:- “Moving to a computer-based system. Previously everything was paper-based, so it took time to get everything online.”
- “Almost a 100% turn around from face-to-face services to Telehealth, within the space of 1 week!”
- “Transitioning clients to Telehealth and helping them manage anxiety about technology.”
- “The initial move to Telehealth and introducing online/contactless payments and forms.”
- “Moving to Telehealth, having to change my whole home office and also making lots of changes so emailing resources is easier. Lots of paperwork!”
- Some also mentioned increased fatigue associated with Telehealth. “I have had to reduce the clients from 6 to 4 per day, and leave a gap between so I can get away from the computer, have a rest or go for a walk.”
- Managing increased demand
For many practitioners, there are new challenges brought about because of the increased demand they’re experiencing. This was identified by many as a key cause of burnout for themselves or their team.- “There are too many clients, everybody is very stressed or unwell, and we have no one to refer to as everyone else is slammed.”
- “The influx of patients, especially couples in crisis, has led to some burnout for me, and I’ve had to set firmer boundaries with myself, take a bit of time off to rest, and turn clients away (which I hate doing).”
- Others noted their biggest challenge as; “dealing with the backlog – we now have the biggest waiting list ever as it wasn’t possible to conduct new assessments via Telehealth.”
- “Our challenge has been triaging patients … we’ve only been able to see those that can’t continue without treatment.”
- Another stated that “the increased demand has made it difficult to manage staff burnout.”
- Uncertainty around government policies
Many health practitioners cited the uncertainty and delays with government announcements as a major challenge. Some of their comments included:- “Being ‘tossed around’ by Government regulations, and unsure whether we could work or not, whether we were part or not part of Allied and essential health has been extremely difficult.”
- “In the early stage, getting last minute notice of changes to Medicare schemes and COVID restrictions, and having to keep redeveloping policies/procedures. The frustration of the Government not extending client access (number of rebated sessions they can access per year, outside lockdown areas) and no notice as yet regarding the extension to Telehealth (or not).”
- “Changes to processes, procedures to cater for changes to Medicare and workers comp. Worked 7 days a week for about 5 weeks to make all the adjustments necessary. Now we’re faced with the potential ending of Medicare rebates for Telehealth. Just about to start changing policies and procedures to ensure clients know it might end but also to manage if it continues. The government seems to delight in giving as little notice as possible.”
- One respondent was moved to say; “It’s not nice to be told you’re ‘non-essential’ when your clients clearly think otherwise!”
- Team & self-management
Another big challenge for private practice owners during this period has been the management of their team. Some comments of this nature included:- “Practitioner fatigue due to heightened diligence and constant fear of infection.”
- “Staff wellbeing and connectedness. Implemented paid recreation break weekly as well as online lunch room daily to encourage social engagement between staff.”
- “The lack of face-to-face appointments is burning out the staff, the rigours of high levels of Telehealth is gruelling on staff and decreases their own job satisfaction.”
- “Losing practitioners/practitioners needing to take stress leave – due to increased stress levels.”
- Others stated their challenge as “staff not wanting reduced hours or pay” or “keeping staff employed, but managed with furlough scheme.”
- Conversely, the opposite is also true, “Getting therapists off Furlough to meet patient demand. Some therapists have reevaluated their lives and don’t want to work as much. I’m recruiting.”
- Recruiting is also proving challenging though with some saying, “it seems there are less people looking for work due to all the government support packages.”
- Of course, the impact of having children at home is also significant – both for solo operators and those with a team:
– “Working from home with school children also at home is difficult. I have spread my sessions out across the week rather than working on my two clinic days only.”
– “Reduced availability to see clients due to children at home so have had to create a waiting list.”
- Managing increased communication
The need for increased client communication as the situation has changed was also cited by many as a major challenge.- One respondent described their biggest challenge as “Efficiently informing clients of changed procedures and protocols. Handled by updating our website regularly, and heavy use of [our practice management system] email communication templates and bulk sending.”
- Personal stress levels
The Coronavirus Pandemic has put a lot of people under extra stress, and of course, this includes allied health practitioners and has implications on their ability to service their clients. Some of their comments related to this include:- “My biggest challenge is meeting the demands of patient care and managing my own self-care whilst juggling family needs. Being able to still work is a blessing but also leaves me feeling exhausted as I have to return home to check on kids and homeschooling plus the usual household activities.”
- “My anxiety – just carrying on is challenging some days.”
- “My challenge is to remain stable emotionally so as to continue to provide a safe place for my patients to address their individual needs.”
- “Maintaining stress levels with clients and self is difficult sometimes. I encourage clients to get outside to exercise and eat healthy. Talk to friends or they can always reach out to me. I exercise and do yoga regularly.”
Many respondents also mentioned the importance of self-care for practitioners during this period. For those that take this seriously, it seems that stress levels can be more easily kept in check. - For example, one respondent said they were focusing on “time management, not working too many hours, preventing burnout. I have taken on a virtual assistant who has taken on the admin side and I have been concentrating on the therapy side.”
- Wearing masks
While no-one objected to the need to wear masks, there are plenty of practitioners who dislike them and find it makes their job more difficult. Especially in certain circumstances.- For example, one practitioner explained that their biggest challenge is the “use of masks by adults in children’s appointments – this creates fear or anxiety in some children and means that facial expressions cannot be easily read.”
- Others reported a big challenge as the “negative impact on people who are hearing impaired and use lip reading”.
- Cleaning protocols
Keeping up with heightened cleaning requirements is also a challenge for many practices.- In particular, one practice owner said, “The cleaning is a nightmare. Everything else has been alright.”
- Keeping informed of changes
Staying abreast of developments and new regulations as they changed has also been a challenge, and has put an extra load on many practitioners.- One solo-practitioner detailed the main challenges to be “keeping up to date and informed with the latest information and protocols in addition to client work and running practice.”
These last two responses sum up the challenges allied health practitioners are facing in their entirety:
“Isolation of therapists, challenges of learning to use Telehealth, loss of contact with vulnerable families, fluctuating morale amongst therapists and families, reduced income and financial hardship.”
“Increased demand for services resulting in longer waitlists and longer wait times, reduced capacity for referring on as other psychologists also full, increased distress in clients, increased mental health load on myself. I am managing my caseload closely – offering screening appointments, providing lists of alternative services, hiring staff.”
Positive Changes for Health Practices as a Result of the Pandemic
On the flip side, practitioners also noted many different silver linings that have come about as a result of the pandemic. When we reviewed the responses, they could be grouped as follows:
- A heightened focus on health
Many practitioners are grateful for the increased focus on health in general, and especially, the increased awareness and recognition of mental health as an important component of wellbeing. Some comments include:- “People’s acceptance and understanding that time invested in themself is ok! Self-care is ok!”
- “My ability to help my clients is better because I look after myself better.”
- Benefits associated with moving online
Although adopting new technologies was listed as one of the major challenges, it also came up repeatedly as a surprising positive outcome of the pandemic. Some of the comments about the best things to come out of the pandemic included:- “Being able to reach clients from outside my area, help people who couldn’t normally get to appointments also via Telehealth.”
- “Growth in acceptance of online therapy, the quick adaptability of technology, and clients’ adoption of it.”
- “Thinking creatively and with innovation and still meeting client needs.”
- “The benefit of Telehealth to many clients.”
- “People are cancelling less – we just make it Telehealth.”
- “Patients have adjusted well to Telehealth.”
- “We are seeing interstate clients not just local.”
- “How well people engaged in Telehealth and how I could still treat trauma this way when it was previously thought not possible.”
- “Telehealth can be a wonderful tool! Reduction in the transmission of general illnesses.”
- “Love working from home and have found Telehealth more effective for some clients.”
- “We can run 90% of services online and worldwide.”
- “Teens like Telehealth!”
- “The flexibility of incorporating Telehealth has been the best thing we’ve done”
- “We had a staff member relocate to another area who has continued to work for us as she can do teletherapy with her clients.”
- “Telehealth has turned out to be a surprisingly effective form of therapy.”
- “Telehealth has helped to grow my business in an area I had previously considered ‘too hard’.”
- “We are now completely paperless!”
- Fewer sick clients
Many practitioners also recognised the benefits of having stricter health policies for attending sessions, as well as the impacts of less community interaction.- “It’s been great not having clients in session who are so sick they should not have come to the session, coughing and sneezing. We’ve had less clinician absences due to illness, because of fewer sick clients and better hygiene.”
- Increased attention to hygiene
Along a similar vein, many practitioners also welcome the new hygiene standards and community awareness:- “Improved hygiene by everyone and caring by all clients regarding safety of fellow clients.”
- A quieter pace
Like many of us, practitioners also found positives in the restrictions, especially with having a quieter pace of life. Some of the silver-linings here included:- “The enjoyment of the work as a result of greater work/life balance.”
- “Making time to rethink my focus and simplify life.”
- “There has been more opportunity for gratitude over small things.”
This sentiment also applied to the way practitioners organise their practice and hours as well. For example: - “Better workday routine with the breaks between patients making the day calmer and less stressful. Would never have thought to do this if it were not for COVID and will not be changing back to the previous routine!”
- “Working remotely has saved a lot of traveling time which has added a lot of efficiency.”
- “I feel less inclined to hustle – and make more time to reflect. I prioritise my own health more now.”
- Community camaraderie
Many health practitioners were pleasantly surprised by the adaptability and compassion shown by their clients.- “Everyone is very understanding and has never had a complaint about being asked to wait outside, or wash hands or cancel because of respiratory symptoms. I feel everyone knows we’re in it together.”
- “I’ve come to realise just how supportive and wonderful my clients are. Not really a change but a wonderful surprise.”
- “People’s resilience and willingness to adapt – both staff and clients.”
- Time to focus on improvements
In addition to moving practice management online, many practitioners also cited a positive as having time to work ON their business, rather than being stuck IN it all the time. Many people explained their positives as:- “This has given me the time to think about how I want to operate and the type of clients I want to take on.”
- “Time to get jobs done that didn’t get time for previously.”
- “I have had more time to research and plan other projects instead of direct client work.”
- “I have changed my appointments to 1 hour from half an hour. Also increased my fees. Patients are very grateful and happy. Plus, it’s very rewarding spending more time with patients.”
- “I have made a lot of changes to the clinic as the 4 months of lockdown allowed me a lot of time to reflect on business practices. We removed the cheaper options for appointments as we did not have the same availability and nearly all clients have just moved up to the more expensive appointment options.”
- “The clinic has had a well overdue clear out and decorate. We’re now a lot more organised.”
- “Our new focus on marketing has increased practice awareness for clients and practitioners alike and resulted in exponential growth in both.”
- “I have enrolled in a coaching program and am looking at new ways to market and develop a signature program to work with clients all over the world in my niche area.”
- “I’ve finally had a chance to rethink my practice. Got off the ‘hamster wheel’!”
- “Something like this makes you reassess your role and assess what’s important… it gives you a bigger picture view.”
- “We now have a cleaner, more organised clinic.”
- “We’ve streamlined our processes and massively reduced the clutter!”
- Increased business opportunities
For some clients, the changes caused by the pandemic have opened up revenue opportunities. For example:- “Something new which may or may not be attributed to the pandemic is that more patients upon completing a series of treatments are requesting continuation of care and monthly follow up. I have been a podiatrist for over 30yrs and I am finding that patients don’t want to end their treatment at the moment. Maybe they find security in me checking in on them on a regular basis.”
Many respondents summed up the surprising positives they’ve experienced as a result of the Coronavirus pandemic:
“We now have increased skills in teletherapy. Plus, we have increased confidence that we are resilient and can cope with changes and respond quickly to new situations. I’m so appreciative of our great team members who have banded together to ensure continued services.”
“The positives have outweighed the negatives in terms of the overall impact on our practice as it has given us the opportunity to be innovative out of necessity with some surprisingly positive results.”
“We are more versatile and more resilient than we imagined, when times change we are able to change with them.”
Ongoing Concerns from Allied Health Practitioners
While the last section highlighted the positive aspects that health practitioners have identified, there are also many concerns for the future – some of which are serious.
Here we’ve provided a cross-section of these:
- Concern for clients and the community
- “Clients being reluctant to attend for face-to-face appointments means that many of them do not get the proper rehab/treatment they normally would and so results are not always as good for the client as they should be. It is difficult to encourage clients that it is safe to attend the clinic even in an area where there is no COVID-19. The loss of employment for many clients also means they are less able to afford to attend as many / any appointments. People are generally a lot more anxious and stressed.”
- “Important to look at the impact of the pandemic on people’s mental health as everyone has suffered from it in some way or another.”
- “Everyone’s stress levels are high. Burnout and fatigue big factors. Dealing with disappointment on repeat.”
- “We see a significant impact on the health of our patients and community – high stress, anxiety, depression, lack of physical activity, lack of social interaction, and the emotional roller coaster are negatively affecting the physiological and physical health of every single person we see, as well as our staff. The risks of the lock-down are far more severe than the risks of actually getting sick from Coronavirus.”
- “The effect of this pandemic on mental health is going to be seen in generations to come. We need to implement support structures now for the future generations that will have mental health diagnosis directly related to the pandemic.”
- Concern for the allied health industry
- “Our industry needs to take some time for self-care.”
- “As the owner of a practice with 6 psychologists and 1 psychiatrist, in 50 years of work as a psychologist, this has been the most intense period of work where I have had to adapt so frequently to changing circumstances.”
- “High practitioner burnout and stress during this time, even where I am where things are relatively stable.”
- “[The COVID Pandemic] takes away our plans, goals and dreams. As an employer, I feel it is harder to provide my staff with the opportunities and aspirations that inspire energy and enthusiasm in their work.”
- “It’s hard being in a caring profession when we need some care ourselves in difficult times.”
- Current sentiment
In addition, the current sentiment of some allied health practitioners is not great, with some responding with things such as:- “I’m tired.”
- “The time spent writing / rewriting policies etc. was the worst. The cleaning sucks. Telehealth is hard. I drink more coffee now.”
- “Just exhausting as a group practice owner. Have had to reduce my own client work substantially to manage burnout.”
- “I’m not sure that I will be able to return to practice and if I do, that my clients will return. It has been a long time of closure.”
- And some practitioners are clearly feeling overworked and under-valued. One mental health professional stated; “While I take nothing away from the doctors and nurses who have been praised for all their efforts during the pandemic, I do feel a little forgotten in the work done by all in the mental health field during the pandemic. We have had to deal every day with the fear, anger, confusion, despair, helplessness and hopelessness people have struggled with over this time without any acknowledgement of how hard this has been when we ourselves have also been grappling with our own personal experience of the pandemic. Who cares for those who have been caring for the mental health of so many many more people throughout this.”
Summary
Clearly, a survey like this also opens up more questions, but hopefully, it provides an insight into the various impacts the Coronavirus Pandemic has had and is still having, on the Allied Health Industry. As we’ve discussed, there have been dramatic impacts on demand levels (varying by allied health profession) and for many practices, it has forced changes in technology adoption, as well as many other changes. The situation over this period has brought about many challenges for allied health practices, as well as some positive outcomes. However, there are many concerns for the future – for practice owners, practitioners, and clients.
Thank You to Respondents
We would like to extend our deepest gratitude to the respondents for taking the time to complete this survey. We hope that knowing the struggles that others are experiencing goes some way to lessen the burden of these difficult times.
About the Coronavirus Impacts Survey
Power Diary surveyed 478 allied health professionals. All of these are in private practice, spanning a cross-section of professions, with most being both practitioners and practice owners. The survey was conducted in September 2020, so these sentiments and findings reflect that point in time.