DAP notes are an important tool used by healthcare professionals to document progress when working with clients. They provide a structured way to keep track of sessions and can be used to create treatment plans, measure progress, and ensure clients receive the best care possible. This article provides useful tips on writing effective DAP notes, as well as practical examples and resources to help you get started.
What Are DAP Notes?
Practitioners use DAP notes to record the progress of a client. It is a structure that standardises how information is recorded in clinical notes so that it makes logical sense to the reader (often, this will be another healthcare provider).
Electronic medical record (EMR) software makes it possible for healthcare providers to digitally document client progress using DAP notes for complete yet concise records that are easily accessible.
Clear, organised DAP notes offer several benefits, including:
- Time-saving: Accessible digital templates provide a framework for what to include in your notes.
- Protection: DAP notes protect practitioners, should a case be reviewed by a standards committee.
- Ease of reference: DAP notes make it easy for other health professionals to review your notes.
- Service excellence: Detailed, accessible records mean you can offer the best care.
- Compliance: DAP notes ensure you stay in line with record-keeping guidelines required by your professional association and country.
Well-written progress notes are also ultimately a reflection of a practitioner’s level of professionalism, so it’s worth ensuring that the method you use to record progress notes is streamlined and efficient.
What Does DAP Stand for?
DAP stands for Data, Assessment, and Plan. When writing a DAP note, each section should build on the previous section, providing a concise summary of the client’s current status, any interventions that have been used, and the client’s progress. Let’s break down these three components in more detail below.
Data
The information in this section should be as factual as possible. In some cases, the information might be self-reported, so you may want to include quotes from the client to illustrate what they’ve said regarding their current condition.
You could also include your own observations but try to keep them unbiased. For example, does the client appear agitated or relaxed? Are they speaking clearly or slurring their words? Examples of factual information include:
- Why the client booked a session?
- The condition of the client – physically and mentally.
- The client’s feedback on events or symptoms since the last session.
- Test results.
- Measures implemented during a session.
Assessment
Here the health practitioner analyses the data that’s been gathered and draws conclusions that are clearly supported by the data. This might include a proposed diagnosis and evaluating the effectiveness of any interventions that have been used so far.
In this section, it’s also important to assess and record the client’s risk for any potential harm. For example, is the client’s mental health deteriorating? Are there any indications of self-harm or suicidal thoughts? This section will form the foundation for the treatment plan, which comes next. Here are some examples of what you might record in this section:
- How a client responded to measures applied in a session.
- How the client’s condition is improving.
- Whether session outcomes are achieved.
- Whether a client’s diagnosis should change.
- Any risks associated with the client’s condition and measures to address it.
Plan
Finally, the health practitioner maps out a plan for upcoming treatment. This should be based on the data and assessment, and include any reasonable interventions that are likely to yield positive results. This section could also include goals for the client, such as improved sleep patterns or better coping strategies.
For example, you might decide to change or add interventions, or perhaps refer the client for additional care. You should also include strategies for follow-up treatment sessions and a timeline for their implementation. The plan section might record details such as:
- Adjustments to the way the client is being treated.
- Instructions and referrals to be given to the client.
- Any additional healthcare practitioners to be involved.
- Details of upcoming sessions (such as the time and date).
What is the Difference Between a DAP Note and a SOAP Note?
DAP notes and SOAP notes are both frameworks used by healthcare professionals to record client progress. The main difference between the two is that a SOAP note breaks down the “Data” in DAP notes into two categories: subjective and objective. In a SOAP note, the “Subjective” section records the client’s self-reported symptoms and how they feel, while the “Objective” section records the clinician’s observations.
Both formats have their merits and provide a valuable, structured way of recording progress when working with clients.
Who Uses DAP Notes?
DAP notes are typically used in the mental and behavioural health fields by HIPAA-compliant psychologists, counsellors, social workers, and other mental health professionals. However, it’s also a framework often used in other disciplines and allied healthcare fields such as general medicine, physiotherapy and occupational therapy, speech-language pathology, chiropractic, and acupuncture.
DAP notes may be required for health services that need documentation of client progress. They can also be used to provide information for billing and insurance reimbursement purposes, as well as other legal requirements. With DAP notes, any practitioner who works with a client can easily review and update their progress.
How to Write a DAP Note
Learning how to write effective DAP notes can be daunting for new practitioners. But with practice and a good understanding of the core principles, you can quickly get the hang of it. Once you become familiar with the structure of a DAP note and have established some templates, you’ll soon find that writing them becomes second nature.
Even if you’re a seasoned practitioner, you still stand to benefit from refreshing and deepening your understanding of the basics. Being able to craft a well-written DAP note will help you provide better care for your clients and make accurate records of their progress. This means that note-taking is a critical skill for any mental health professional. It’s a skill you should hone until you’re confident in your ability to produce succinct, accurate DAP notes.
The following includes tips on how to write an effective DAP note.
Tips for Writing Effective DAP Notes
- Focus on simplicity and clarity: It’s important to decide what information you want to include in your DAP note as a rule and what you want to leave out. The point is to record helpful information only. The length of your DAP note will depend on how well a client is progressing. The note may be longer when a client doesn’t progress as expected.
- Understand your intended outcome: Determine the format of your progress notes by imagining that you’re reading a DAP note written by someone else. What would help you scan it and understand the information well? Perhaps short key phrases in one section and a numbered list in another?
- Use robust software to stay organised: Using electronic software like Power Diary to record your DAP notes will help you navigate to important information quickly. While you could use a DAP note template, then write it by hand and upload it to the software, recording the DAP note directly into the software is more efficient and accurate. In addition, well-designed software can add value to your notes with elements like charts and checklists.
- Be mindful of who will read them: DAP notes are not your personal diary – they are professional documents that may be reviewed by other practitioners or even a court. As such, it’s important to be mindful of what you write and avoid any assumptions, language, or unnecessary details that could affect the client negatively or demonstrate personal bias. This also means you should always write the notes in a way that is easy to understand for anyone who reads them.
- Consider modifying your DAP notes: While the structure of a DAP note typically never changes, there may be times when you need to adapt some elements depending on the client’s situation. For example, some mental health practitioners find it helpful to include a “response” section, which records the client’s response to any proposed treatments or strategies.
- Don’t delay writing your DAP notes: You may be in the habit of postponing fully completing your DAP notes until after the client session so that you can give them your full attention. However, it’s important to take the time immediately after a session to jot down every piece of information that you feel is relevant or important to include in your final DAP notes. If you delay writing your notes, you risk forgetting details or misconstruing information.
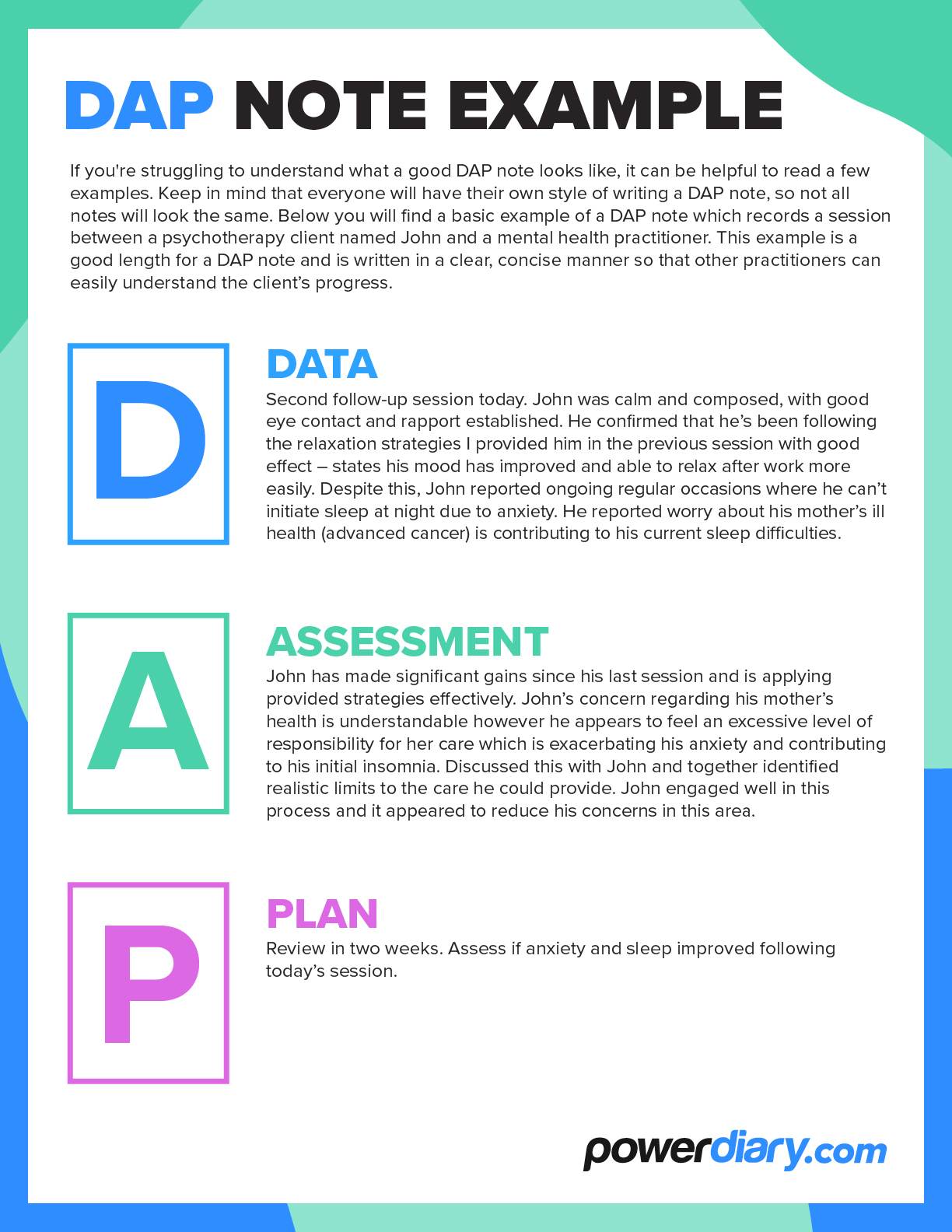
DAP Note Example
If you’re struggling to visualise what a good DAP note looks like, it can be helpful to read a few examples. Keep in mind that everyone will have their own style of writing a DAP note, so not all notes will look the same. Below you will find a basic example of a DAP note which records a session between a psychotherapy client named John and a mental health practitioner. This example is a good length for a DAP note and is written in a clear, concise manner so that other practitioners can easily understand the client’s progress.
Data
“Second follow-up session today. John was calm and composed, with good eye contact and rapport established. He confirmed that he’s been following the relaxation strategies I provided him in the previous session with good effect – states his mood has improved and able to relax after work more easily. Despite this, John reported ongoing regular occasions where he can’t initiate sleep at night due to anxiety. He reported worry about his mother’s ill health (advanced cancer) is contributing to his current sleep difficulties.“
Assessment
“John has made significant gains since his last session and is applying provided strategies effectively. John’s concern regarding his mother’s health is understandable however he appears to feel an excessive level of responsibility for her care which is exacerbating his anxiety and contributing to his initial insomnia. Discussed this with John and together identified realistic limits to the care he could provide. John engaged well in this process and it appeared to reduce his concerns in this area.“
Plan
“Review in two weeks. Assess if anxiety and sleep improved following today’s session.“
Improve the Note Writing Process with EMR Software
EMR software like Power Diary speeds up your note-taking and ensures that your notes contain helpful information with a logical layout. The software lets you create a DAP note template that suits your specific needs. This capability will be right at your fingertips if you need different templates for a first meeting, a follow-up phone call, sequential sessions, and more.
What Is EMR Software?
EMR stands for electronic medical records. EMR software helps healthcare providers streamline workflows in their practice, from booking appointments and automating appointment reminders for clients to recording client information, including their details and medical records and invoicing.
Choosing EMR Software for DAP Notes
Different healthcare professionals will benefit from different features offered by EMR software. Before making a decision on EMR software for your practice, you should ask the following questions:
- Does the software offer all the features you need?
- Is there a pricing structure that lets you pay a competitive rate corresponding to the size of your practice?
- Are all the required features included in the pricing option that you want?
- Is the software well suited to the industry you’re in?
- Will you be getting the best value for money?
Look at online reviews, check out our excellent G2 and Trustpilot ratings, or sign up for a free trial of Power Diary to start using the software today.
Beneficial Features of Power Diary
Power Diary simplifies life for both healthcare providers and their clients with these outstanding features:
- Customisable templates for DAP notes
- An all-in-one solution that links all aspects of the client’s information
- Online bookings with configurable forms for data collection and client consent
- Different ways to connect with clients and check in with them or send appointment reminders
- Management of all a client’s information and history without the need to leave the system
- Hassle-free integrations with complementary software
- Simple calendar management that includes a waiting list function
- The functionality to conduct secure, in-platform telehealth sessions
- Safe ways to pay and sophisticated management of outstanding accounts
- An affordable and flexible pricing structure designed to suit any practice size
Make DAP Notes More Efficient with Power Diary
Not all practice management systems are created equal. Some don’t provide enough flexibility for customised DAP note templates but Power Diary is different. Co-founded by a psychologist, it’s been pressure-tested to meet the specific needs of healthcare professionals and streamline their workflows.
Power Diary makes DAP note creation easier and faster, so you can spend less time on paperwork and more time providing quality care for your clients. It’s the fastest way to boost client care and uplift your entire practice from the inside out. Try it out today with a free trial or demo and experience the benefits first-hand.