SOAP notes are a clinical note format that serves as a blueprint for documentation in occupational therapy. These notes have a dual purpose–as a historical record and as a guide to therapeutic decision-making.
That’s why accurate and efficient SOAP note-taking is the backbone of effective therapy.
Ready to hone your SOAP note game?
Let’s explore how to draft notes so every word contributes to your patient’s progress.
Understanding SOAP Notes in Occupational Therapy
What Does SOAP Stand For?
SOAP stands for Subjective, Objective, Assessment and Plan.
SOAP notes are a standardized method of documentation used by healthcare professionals. In occupational therapy, these notes serve as a communication tool for recording the details of each session, contributing to continuity and consistency in patient care.
History of SOAP Notes in Occupational Therapy
The SOAP note format has its roots in the medical field and has evolved over time to become widely used across multiple healthcare professions, including occupational therapy.
Originally developed in the 1960s by Dr. Lawrence Weed, SOAP notes were designed to provide a clear, concise, and systematic way of documenting patient care. In occupational therapy, this format is used and adapted to meet the specific needs of the field.
Over time, SOAP notes have evolved to not only document patient encounters but also to facilitate holistic treatment planning, collaboration among healthcare professionals and help ensure compliance with legal and ethical standards.
The Role of SOAP Notes in Treatment Planning & Progress Tracking in Occupational Therapy
In occupational therapy, writing effective SOAP notes is essential to treatment planning and progress tracking.
SOAP notes help occupational therapists:
- Develop and adjust treatment plans
- Track progress over time
- Enhance communication between therapists, healthcare providers and insurance companies
- Maintain legal and ethical standards
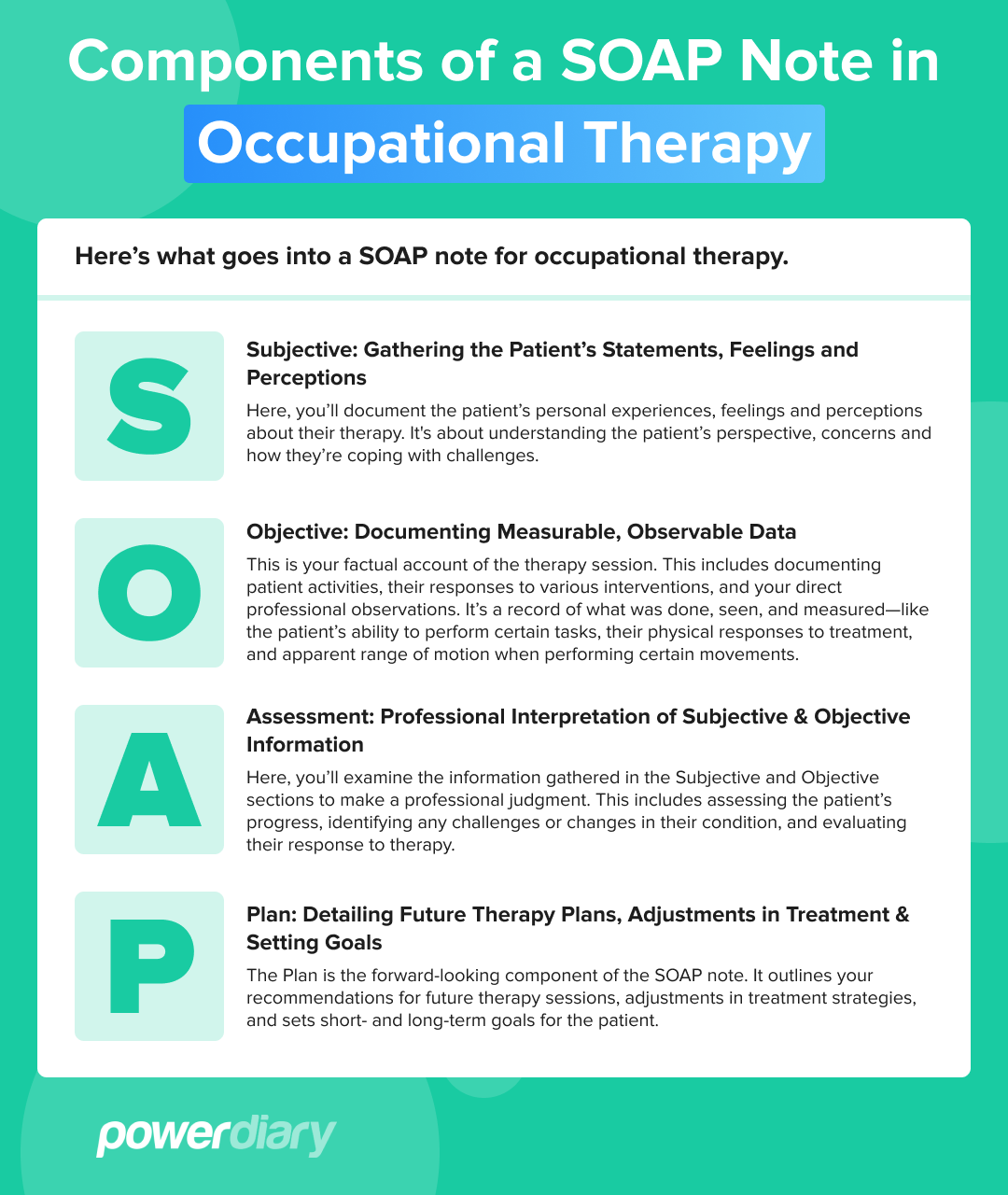
The Components of a SOAP Note in Occupational Therapy
One of the great successes of the SOAP note format is that its structure is adaptable across many different healthcare disciplines.
But it’s worth examining SOAP note components in the specific context of occupational therapy.
Let’s take a look:
Subjective: Gathering the Patient’s Statements, Feelings and Perceptions
Here, you’ll document the patient’s personal experiences, feelings and perceptions about their therapy. It’s about understanding the patient’s perspective, concerns and how they’re coping with challenges.
Objective: Documenting Measurable, Observable Data
This is your factual account of the therapy session. This includes documenting patient activities, their responses to various interventions, and your direct professional observations. It’s a record of what was done, seen, and measured – like the patient’s ability to perform certain tasks, their physical responses to treatment, and apparent range of motion when performing certain movements.
Assessment: Professional Interpretation of Subjective & Objective Information
Here, you’ll examine the information gathered in the Subjective and Objective sections to make a professional judgment. This includes assessing the patient’s progress, identifying any challenges or changes in their condition, and evaluating their response to therapy.
Plan: Detailing Future Therapy Plans, Adjustments in Treatment & Setting Goals
The Plan is the forward-looking component of the SOAP note. It outlines your recommendations for future therapy sessions, adjustments in treatment strategies, and sets short- and long-term goals for the patient.
SOAP Note Examples Occupational Therapy
To provide a practical understanding, let’s look at some hypothetical examples:
OT SOAP Note Example 1
- Subjective: The patient states she hasn’t been able to use her wheelchair for almost two months as her “hands hurt” and “I’m not able to get a good grip.” Patient mentions “feeling overwhelmed”.
- Objective: Mild tenderness upon palpation of the client’s palms. Grip strength 36 lbs.
- Assessment: Possible peripheral neuropathy, possible cervical compression. Differential diagnosis allows for potential Parkinson’s or arthritis.
- Plan: Commence strengthening, stretching, and motor-coordination exercises twice weekly, and provide the client with a schedule of home exercises for maintenance. Arrange relevant blood tests to confirm or rule out peripheral neuropathy diagnosis.
OT SOAP Note Example 2
- Subjective: The patient stated, “I feel awkward in gym class, especially during team sports. I just can’t seem to keep up with others.”
- Objective: The patient displayed coordination difficulties during ball-catching exercises and appeared hesitant in movements requiring quick changes in direction. Reaction time was slower compared to peers of a similar age.
- Assessment: The patient shows signs of developmental coordination disorder, impacting their physical abilities in fast-paced activities. This difficulty contributes to a lack of confidence in social and physical activities, particularly noticeable in group settings like gym class.
- Plan: Develop a plan to improve coordination and reaction time through specific exercises, such as catch-and-throw activities and agility drills. Additionally, introduce confidence-building exercises and strategies for coping with anxiety in social situations. Establish a short-term goal for the patient to participate more actively in gym class within the next six weeks.
Best Practices for Effective SOAP Notes in Occupational Therapy
Writing SOAP notes in occupational therapy requires clarity, accuracy and efficiency.
Tips for Clarity, Accuracy & Efficiency in Note-Taking
- Clear and concise language: Use straightforward and precise language to avoid ambiguities. Avoid jargon and use universal abbreviations (if any) for ease of understanding by other healthcare professionals.
- Document observable and measurable data: In the Objective section, include factual information such as treatment details, your observations and measurable results. Focus on skills rather than just activities performed.
- Functional goals: Your plans should include specific, measurable, achievable, relevant and timely (SMART) goals. This makes it easier to track progress and adjust treatment strategies accordingly.
- Strength-based language: Focus on the patient’s strengths and achievements. This positive framing can boost the therapeutic relationship and patient morale, especially if patients ask to review their notes.
- Patient-centered language: Ensure that your notes revolve around the patient’s needs and goals. Describe interventions in terms that are meaningful to the patient.
- Regular updates: Update your SOAP notes to reflect changes in the patient’s condition and therapy adjustments. This helps in tracking the effectiveness of your interventions.
- Compliance and legibility: Adhere to all applicable legal and regulatory standards for documentation. Ensure your notes are legible, complete and use standard terminology for consistency.
- Practice management system: Implementing an effective practice management system can streamline documentation and note-taking, reduce errors and facilitate secure, easy access to patient data.
Ethical & Legal Considerations for Occupational Therapy SOAP Notes
As in other healthcare disciplines, confidentiality and privacy are paramount in occupational therapy. Therapists are entrusted with sensitive information about their patients’ health, personal lives and progress. Therefore, occupational therapy professionals must safeguard all forms of communication – whether written, verbal or electronic.
Legal Implications & Standards in Documentation
Occupational therapists must adhere to all relevant policies, guidelines and regulations regarding confidentiality. This includes understanding and complying with laws like HIPAA, which sets standards for protecting health records.
Violations of privacy regulations can lead to legal consequences and are considered professional misconduct.
Navigating Sensitive Patient Information in SOAP Notes
Handling sensitive patient information in SOAP notes requires a careful and ethical approach.
Occupational therapists should:
- Use clear and respectful language: Avoid judgmental language. Be objective and professional in describing the patient’s condition and progress.
- Be mindful of what to include: Only include information relevant to the patient’s treatment and progress. Avoid unnecessary details that don’t contribute to therapeutic goals.
- Secure storage and transmission: Ensure that all SOAP notes and patient records are stored securely, whether in physical files or in electronic formats. Use encrypted channels for transmitting sensitive information.
- Consent and release of information: Always obtain consent from the patient or their guardian before sharing any information. Be clear about what information will be shared, with whom and for what purpose.
- Regular updates on regulations: Stay informed about changes in legal and ethical guidelines related to documentation in occupational therapy.
- Technology and security: When using electronic systems for documentation, ensure that they comply with relevant security standards and protect patient data effectively. Secure systems like Power Diary are ISO 27001-compliant and compliant with major regulatory bodies.
- Professional training and development: Regularly update your knowledge and skills regarding ethical and legal aspects of documentation through professional development opportunities and resources.
Practical Tips & Common Pitfalls
Tips for New Practitioners in Occupational Therapy
- Client-centered approach: Always keep the patient as the focus of your documentation. Remember, in the story of therapy, the patient is the hero, and you are the guide.
- Use of abbreviations: While abbreviations save time, ensure they’re universally understood. Avoid cryptic or specialty-specific abbreviations that might confuse other healthcare providers.
- Create a documentation cheat sheet: Develop a template or cheat sheet. This can be a list of power words or a fictional note example, adjusted to your style and setting.
- Consistency: Be consistent in your documentation style. This helps other healthcare providers understand the patient’s progress and treatment plan easily.
- Timely note-taking: Don’t delay drafting your SOAP notes. This helps ensure your notes are accurate and complete when logging data into the patient’s records.
- Leverage technology: Use practice management software for efficient note-taking. The right software will support and advance your record-keeping efforts, and an in-platform template library can give you a head start. It’s essential to choose software that is user-friendly and aligns with the specific needs of your practice.
Common Mistakes in SOAP Note Documentation
Below, we’ve listed a few common mistakes made in occupational therapy SOAP notes. Fortunately, they’re easy to avoid.
Mistake #1: Waiting to Record Your SOAP Notes
- Mistake: Putting off drafting your SOAP notes until the end of the day. This raises the chances of inaccuracies or omissions in your SOAP notes, especially when you’ve seen many patients.
- How to avoid it: Use a SOAP note template and take 10 minutes after each session to download your professional impressions. This not only ensures greater accuracy, but will lighten your load and help prevent the overwhelm of trying to accurately capture multiple patients’ notes at the end of each day.
Mistake #2: Repeating Information in the Assessment Section
- Mistake: You repeat the information contained under the Subjective and Objective sections in the Assessment section.
- How to avoid it: Pay attention to the purpose of each section. The Assessment section is designed to accommodate your professional interpretation of the presenting problem, based on what the patient reports and the observable data you gather; it’s not designed for further observations or patient-reported symptoms.
Mistake #3: Using Vague Language
- Mistake: You make general statements or are too brief in your descriptions under the Subjective and Objective sections.
- How to avoid it: Be specific and avoid vague statements. You shouldn’t write paragraphs of unnecessary information. Include all measurable data, specifics of the interventions and the patient’s responses to them.
Integrating SOAP Notes into Daily Practice
By integrating a few good strategies into daily practice, occupational therapists can efficiently manage SOAP note documentation:
- Develop a routine: Establish a routine for writing SOAP notes. For example, this might mean scheduling time immediately after each session for note-taking.
- In-session note-taking: Develop a habit of taking brief notes during sessions. This can include jotting down key subjective statements from the patient or significant objective observations, making the post-session documentation process smoother.
- Use templates and checklists: Use templates or checklists based on the SOAP format. This ensures all necessary information is covered without having to start from scratch each time.
- Client involvement: Involve patients in the documentation process where appropriate, such as confirming goals or subjective experiences. This can enhance the accuracy of the information and save time.
Balancing Detailed Documentation with Time Constraints
- Make key information a priority: Focus on documenting the most critical information that reflects the patient’s progress and your clinical reasoning. Avoid getting bogged down by unnecessary details.
- Efficient writing techniques: Use bullet points or short phrases instead of long sentences where appropriate. This approach can save time while still providing necessary details.
- Leverage technology: Use speech-to-text to expedite the documentation process.
- Time management: Allocate specific time slots for documentation within your daily schedule. Consider this as a crucial part of patient care, not just an administrative task.
Continuing Education for SOAP Notes
- Professional development: Engage in learning opportunities such as workshops, webinars, or courses focused on documentation skills.
- Stay informed about industry changes: Keep up-to-date with any changes in documentation standards or best practices in occupational therapy. This ensures that your SOAP notes always meet the current professional and legal requirements.
- Reflective practice: Regularly review your own SOAP notes to identify areas for improvement. Reflect on what works well and what can be improved in your documentation process.
- Adapt to patient needs: Be flexible in your documentation approach to suit different patient needs and scenarios. This adaptability is essential for providing effective therapy.
Conclusion
For occupational therapists, mastering the art of SOAP note-taking requires continuous learning and reflection.
Power Diary is designed with the needs of occupational therapists in mind, providing an all-in-one practice management platform. By choosing Power Diary, therapists can focus more on patient care, and less on administration.
Start with a 14-day FREE TRIAL – no credit card required – and discover how seamless and efficient your documentation process can be.