If you’re an allied health practitioner, you’ve likely heard about SOAP notes. After all, it’s a widely used method for clinical note documentation that’s been around for nearly 50 years.
But, there’s often not much guidance about what to include and how best to go about writing them.
Getting your SOAP notes right is important because effective healthcare documentation is imperative to enhance client outcomes and avoid unwanted consequences.
And SOAP notes have a significant role to play.
SOAP notes help practitioners capture the whole picture of a client’s journey over time, from intake to treatment.
Whether you’re a seasoned practitioner or new to the field, mastering this skill is essential. And when you do, it will save you loads of admin time!
Understanding SOAP Notes
SOAP notes are a tool for documenting what the client says, what the allied health practitioner observes, the diagnosis or assessment, and the plan for the client’s care.
As common as this note-taking style has become, you might be wondering about the format’s origins and how it stacks up against other note-taking conventions.
Definition & History of SOAP Notes
SOAP stands for Subjective, Objective, Assessment, and Plan (in that order). It’s a method of note-taking that allied health professionals use to record and review ongoing client care.
SOAP notes were introduced in the 1960s by Dr. Lawrence Weed, known for his work in medical record standardization. His vision was to improve the quality of client care by creating standard client documentation systems – and the success of his pioneering is evident in the broad use of SOAP notes in allied health today.
The Purpose & Significance of SOAP Notes in Client Care
SOAP notes are a documentation tool that helps ensure clinical notes are recorded accurately and addressed with an appropriate treatment plan.
The SOAP format provides structure and guides practitioners through each of the necessary elements of quality clinical documentation.
SOAP vs Other Types of Clinical Notes
While SOAP notes are widely used, they’re not the only option for clinical documentation.
Other types of clinical notes include DAP (Data, Assessment and Plan) and GIRP (Goals, Interventions, Response and Plan), among others. Each type of note has its place in client care.
Like SOAP notes, DAP notes focus largely on the data gathered during the client’s visit.
GIRP notes, on the other hand, focus on the client’s goals, the interventions used by the clinician, the client’s response to these interventions and the plan moving forward.
The Components of a SOAP Note
Let’s break down each component of a SOAP note, with examples to bring them to life.
Subjective: Gather the Client’s History and Statements
The ‘Subjective’ component is the storytelling part. It’s where the client shares their symptoms, feelings and personal experiences.
This section is purely from the client’s perspective, like a narrative of their health journey. For instance, a client might say, “I’ve been feeling really anxious lately and having trouble sleeping.”
This subjective information is invaluable as it gives insight into the client’s experiences and concerns, and gives context for the Assessment and Plan stages.
Objective: Document Observable and Measurable Data
This part is all about measurable, observable data that the healthcare provider gathers during the examination.
This includes vital signs, affect, physical exam findings, and any other concrete data. For example, “The client’s blood pressure is 140/90 mmHg, and heart rate is 98 bpm.” This data provides a factual basis for the assessment and plan.
Mental health practitioners may record mental state examination data in this section as well.
Assessment: Practitioner’s Diagnosis or Impression of the Client’s Condition
Assessment is where the allied health practitioner submits their professional opinion. Based on the subjective and objective information, they formulate a clinical judgement.
This could be a diagnosis, a list of possibilities, or an impression of the client’s condition. For instance, “The symptoms are consistent with an anxiety disorder.” This part connects the dots between what the client experiences and what the practitioner observes.
Plan: Outline of Treatment and Management Plan for the Client
Finally, the ‘Plan’ stage is the roadmap for the future. It outlines the treatment and management strategy for the client.
This could include medications, therapies, lifestyle changes or referrals to specialists. A plan might read, “Start a low-dose anti-anxiety medication, schedule weekly sessions and book a follow-up in two weeks.” The plan is all about action and next steps.
Best Practice for Writing SOAP Notes
Writing effective SOAP notes is about balancing detail with clarity and ensuring each note serves its purpose in client care. Let’s explore some best practices.
Clarity, Conciseness & Coherence
Other healthcare practitioners may need access to your SOAP notes when clinically necessary, so notes must be recorded in a professional voice – this is where clarity, conciseness and coherence play a vital role.
For clarity, use simple and direct language – and avoid industry jargon. If using abbreviations, spell it out in full at the first mention and then indicate its abbreviation in parenthesis.
You’ll achieve conciseness by employing brief but comprehensive descriptions. Include all relevant information, but avoid unnecessary details.
And last but not least – coherence is crucial. Each part of the SOAP note should flow logically into the next. The Subjective and Objective sections set the scene, the Assessment connects the dots and the Plan maps out the next steps.
Importance of Maintaining Client Confidentiality
When drafting SOAP notes, always adhere to any relevant privacy regulations and requirements, such as HIPAA or AHPRA, and your practice’s own privacy policies.
This means storing SOAP notes securely and ensuring they’re only accessible to approved personnel. Remember – not only is maintaining confidentiality imperative to foster trust with your client – a breach of confidentiality can have serious legal and ethical consequences.
How To Avoid Common Mistakes
In our experience, these are the most common mistakes to be aware of when drafting SOAP notes:
- Ambiguous language and assumptions – Stick to the facts. Precision aids professionalism. This is especially important in the Subjective section, where the client’s own words should be used – don’t elaborate or create unrelated interpretations.
- Illegible handwriting – Here’s another reminder that other allied health professionals may need access to your SOAP notes at some point. Not everyone has impeccable handwriting, but paying attention to legibility is one of the simplest ways to keep your SOAP notes professional.
- Neglect of suicidal ideation – It’s essential for practitioners to note any suicidal thoughts, feelings, or intentions that clients may disclose during sessions. This should be noted in detail as it’s important for the practitioner to identify any potential risk factors and provide appropriate care. Even if no suicidal risk factors are present it is important to document this in the mental health notes as it demonstrates the therapist has assessed this.
- Breaching client confidentiality – Mental health notes should never be shared or discussed with anyone outside of a session without the express written consent of the client. To maintain client confidentiality, notes should remain secure at all times.
- Failing to comply with legal requirements – Mental health notes should always be taken in accordance with the relevant laws and regulations of the practitioner’s jurisdiction. Failing to do so can lead to legal issues for the practitioner and their business.
- Confusing shorthand – If your writing can’t be easily deciphered by another practitioner, it doesn’t belong in your SOAP notes. Bear in mind that SOAP notes need to serve your client’s best interests – if future health professionals can’t decipher your notes, then they haven’t served their purpose.
The Role of SOAP Notes in Continuity of Care
SOAP notes are tools for continuity of care. They help to ensure that any healthcare provider who picks up a client’s file can understand their history and current plan.
More than that, effective and compliant SOAP notes help protect allied health practitioners against the risk of inconsistency or allegations of malpractice.
This is where Power Diary can be a game-changer, offering configurable note templates and secure access to client notes. You can even write SOAP note best practices into your in-platform Practice Operations Manual.
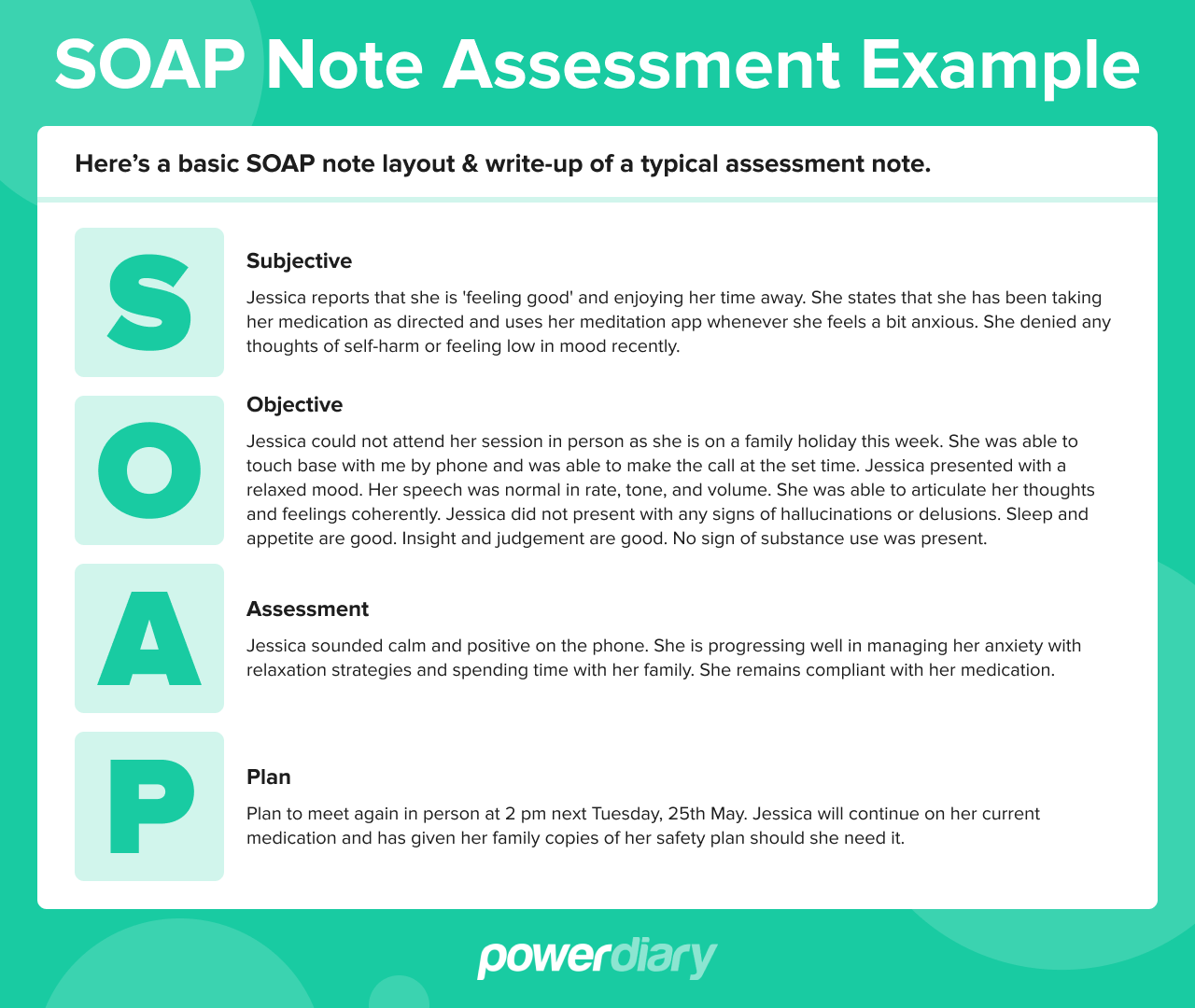
SOAP Note Assessment Example
Here’s a basic SOAP note layout and write-up of a typical assessment note.
Subjective
Jessica reports that she is ‘feeling good’ and enjoying her time away. She states that she has been taking her medication as directed and uses her meditation app whenever she feels a bit anxious. She denied any thoughts of self-harm or feeling low in mood recently.
Objective
Jessica could not attend her session in person as she is on a family holiday this week. She was able to touch base with me by phone and was able to make the call at the set time.
Jessica presented with a relaxed mood. Her speech was normal in rate, tone, and volume. She was able to articulate her thoughts and feelings coherently.
Jessica did not present with any signs of hallucinations or delusions. Sleep and appetite are good. Insight and judgement are good. No sign of substance use was present.
Assessment
Jessica sounded calm and positive on the phone. She is progressing well in managing her anxiety with relaxation strategies and spending time with her family. She remains compliant with her medication.
Plan
Plan to meet again in person at 2 pm next Tuesday, 25th May. Jessica will continue on her current medication and has given her family copies of her safety plan should she need it.
Legal & Ethical Considerations of SOAP Notes
Understanding the legal and ethical dimensions of SOAP notes is crucial for any allied health professional.
Legal Implications of SOAP Notes in Client Care
SOAP notes can play a role in legal scenarios, such as malpractice lawsuits or insurance claims. They provide a clear, time-stamped record of client care. It’s essential to ensure that notes are accurate, timely and complete.
A key factor is adherence to regulatory standards. SOAP notes should comply with laws and regulations governing client records. This includes following guidelines for documentation and records retention.
Ethical Guidelines for Documenting Sensitive Client Information
SOAP notes often contain sensitive data, and the allied health practitioner has a responsibility to protect this information.
This means being vigilant about who has access to notes and how they’re stored and shared.
When documenting sensitive information, it’s important to be respectful and non-judgmental. The language used should be professional and focused on the client’s care and well-being.
Finally, be especially aware of the regulations in your federal or national jurisdiction – it’s the difference between running a thriving and compliant practice and reputational damage.
Power Diary Security Certifications
The security of electronic health records like SOAP notes is essential.
Designed with robust security measures to protect sensitive client information, Power Diary is ISO 27001-certified. Moreover, the software is HIPAA-compliant and GDPR-compliant. It’s also an Australian Cyber Security Centre Partner and is compliant with the Australian Privacy Act. Last but not least, Power Diary is POPIA-, CCPA-, and PIPEDA-compliant. The software’s adherence to international privacy laws ensures that data is handled with the utmost care.
Integrating SOAP Notes into Clinical Practice
Now that we’ve covered the fundamentals and best practices for SOAP notes, let’s focus on integrating them into your clinical practice.
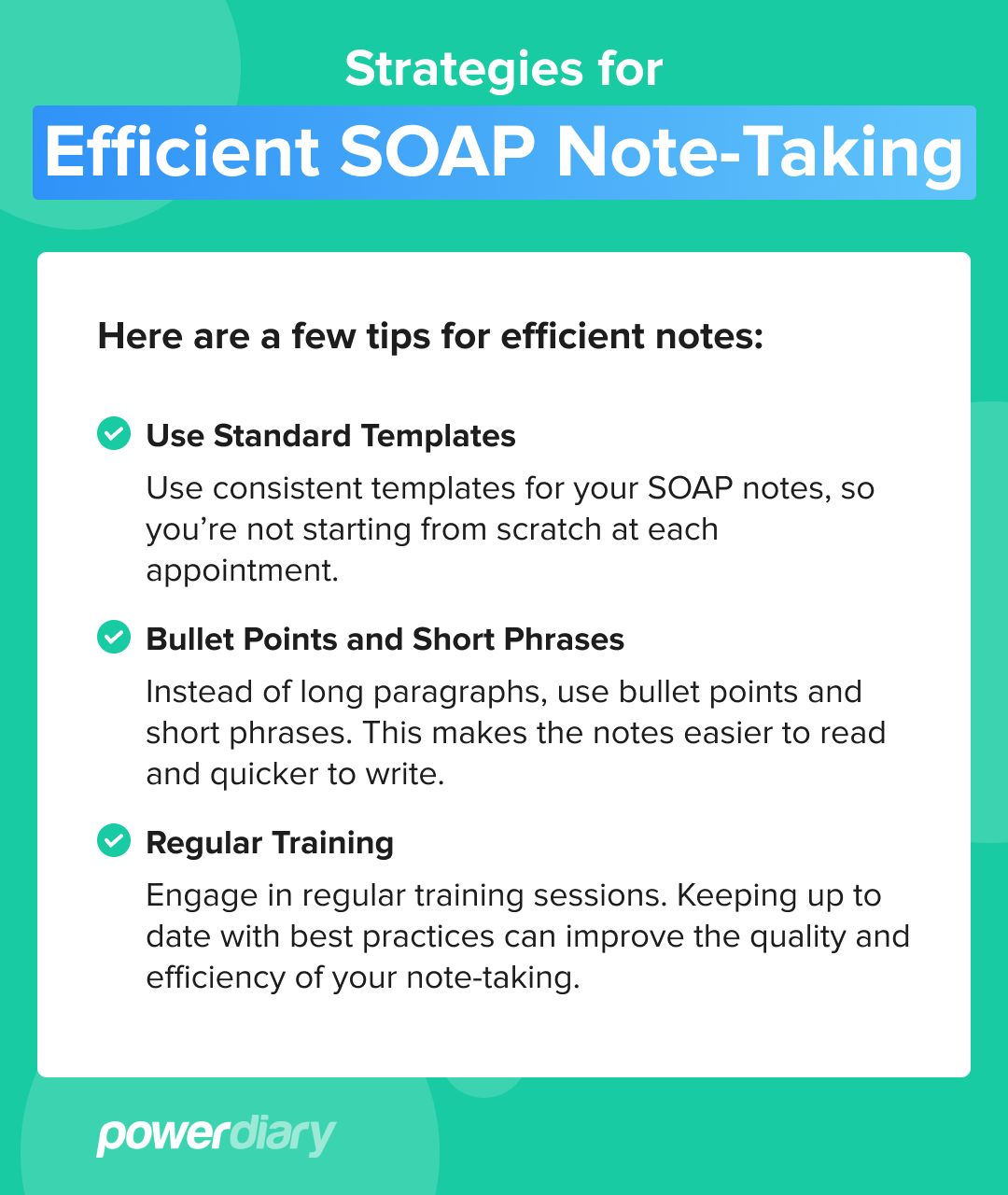
Strategies for Efficient SOAP Note-Taking
Here are a few tips for efficient notes:
- Use Standard Templates: Use consistent templates for your SOAP notes, so you’re not starting from scratch at each appointment.
- Bullet Points and Short Phrases: Instead of long paragraphs, use bullet points and short phrases. This makes the notes easier to read and quicker to write.
- Regular Training: Engage in regular training sessions. Keeping up to date with best practices can improve the quality and efficiency of your note-taking.
The Role of Technology in SOAP Note Documentation
Electronic health records (EHRs) and practice management software like Power Diary offer intuitive, secure platforms for creating, storing and managing clinical notes.
Features like configurable templates, easy access to client information and secure data storage make technology indispensable in today’s healthcare practices.
Training & Resources for Healthcare Professionals
Ongoing training and access to quality resources are essential for mastering SOAP notes. Power Diary provides resources to help healthcare professionals write clinical notes more efficiently.
Depending on your allied health discipline, there are many professional bodies offering further training on clinical note-taking. Incorporating professional development into your practice not only enhances the quality of SOAP notes but also helps ensure your documentation process is as efficient and effective as possible.
Conclusion
From understanding the subjective experiences of clients to documenting objective data, assessing conditions, and planning for care, we’ve covered the ins and outs of SOAP notes in client care.
Technology, particularly platforms like Power Diary, can transform the way SOAP notes are created, stored and used, making them more efficient and secure. To empower your practice in this vital area, consider Power Diary. With a 14-day free trial – no credit card required – it’s an opportunity to experience firsthand how the right tools can enhance the quality and efficiency of your SOAP notes.