As a speech pathologist, it’s important that your SOAP notes are well-structured, accurate, comprehensive, and helpful for both you and your client. This helps ensure that clients receive the best care possible, making your job easier. But when you’re juggling multiple responsibilities, note-taking can suffer. Fortunately, with the right approach, it’s possible to ensure that your SOAP notes are of the highest quality.
What Is a SOAP Note in Speech-Language Pathology?
SOAP notes are widely used for documenting the progress and treatment of clients in various healthcare fields, such as general practice, mental health, and speech therapy. SOAP notes provide a structured format to succinctly document a client’s information, such as reported symptoms and concerns, observations from the clinician, any measurable data, an assessment of the client’s condition, and a plan for treatment moving forward.
Your SOAP notes not only serve as a record of the client’s progress, but they also help to communicate important information to other healthcare team members. Whether you’re a seasoned speech therapist or just starting out, understanding how to write effective SOAP notes is essential to providing top-notch care to your clients.
Recommended SOAP Note Format for Speech Therapy Clinics
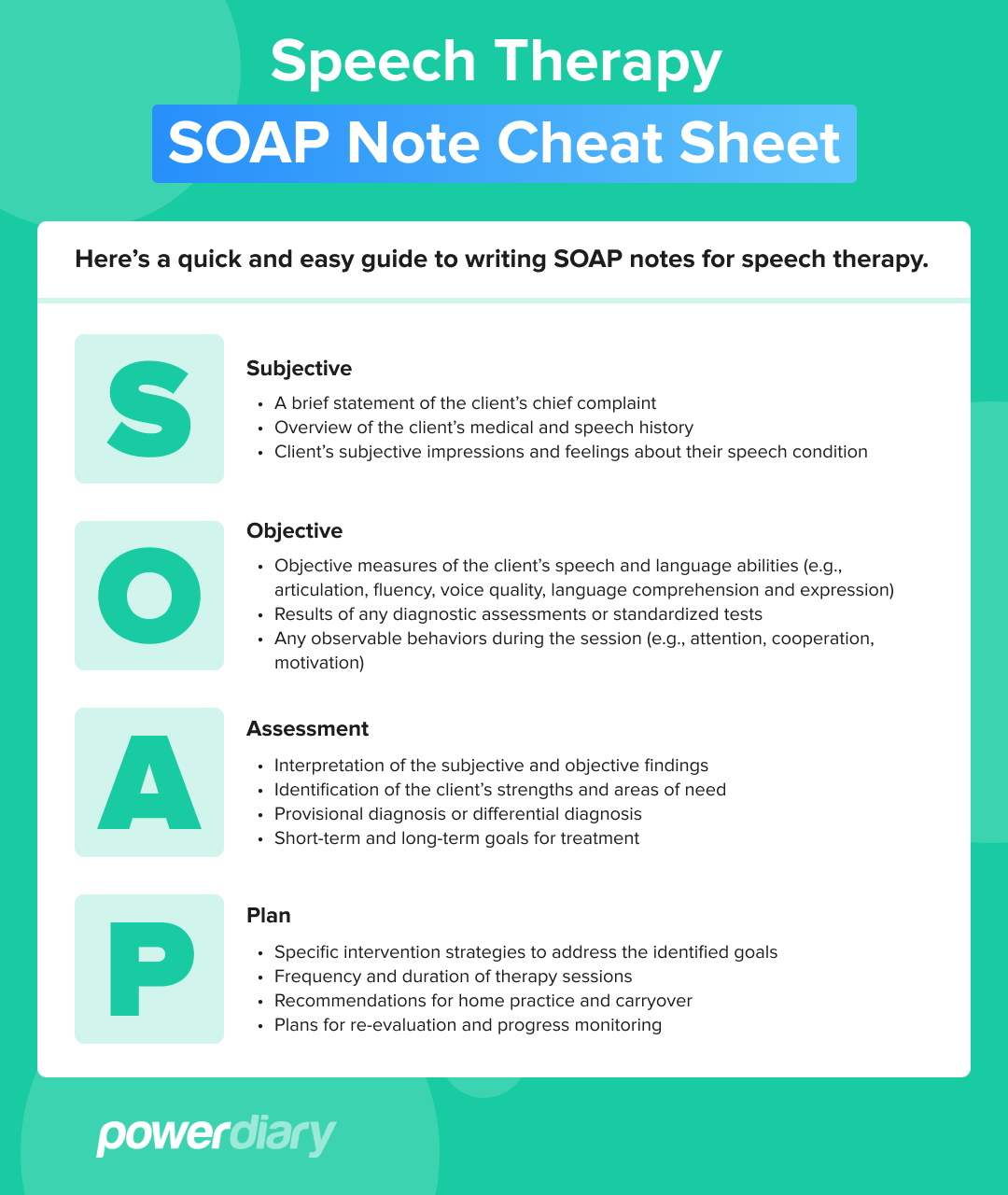
SOAP stands for Subjective, Objective, Assessment and Plan. These four components of a SOAP note provide a framework for the documentation of speech therapy sessions. In the sections below, we’ll go into more detail about each element.
Subjective
This section is all about what the client is experiencing. It should address client concerns, symptoms, and any other relevant information reported, including the history of treatment, current lifestyle, and any external factors affecting the client.
While this section may contain subjective observations of the client’s mood and demeanor, try to keep things as factual as possible. For example, rather than saying, “The client seemed anxious.” you could say, “The client reported feeling anxious.”. You should also record any medications the client is currently taking.
Objective
When writing the objective section of a SOAP note, you should document any measurable or observable information you’ve gathered during your assessment. This includes data such as physical examination findings, vocal range articulation and vocal quality. Record the results here if you perform tests such as a standardized assessment, an audiogram or a hearing test.
Assessment
This part of your SOAP note should include a summary of your observations and an analysis of the client’s condition. If you come to any conclusions or diagnoses, make sure to include these. This section should be detailed and provide a clear framework for the rest of your note.
Plan
Finally, the plan section will include your proposed treatment plan. This could involve regular therapy sessions, advice on lifestyle changes, recommended exercises or any other interventions you deem necessary. Also include how you’ll review the client’s progress, and what goals you have for them to achieve.
How to Write SOAP Notes for Speech Therapy
Here are a few handy tips to help you get started:
Use a SOAP Note Template
Using a template for SOAP notes can help you write clear and consistent notes, saving time by allowing you to fill in the necessary information quickly. By using the same template for all your notes, you can ensure that each note contains the necessary information and is easy to read.
A template also helps to keep your notes cohesive. This provides a consistent structure for all of your SOAP notes, making them easier for other team members to follow and understand.
Be Overly Descriptive
You might be tempted to shorten and quickly sum up your notes to save time – don’t do it! It’s crucial to be detailed and descriptive when writing SOAP notes for speech pathology. It will help you provide a comprehensive overview of the client’s progress.
It’s better to over-explain than to under-explain. Your notes should include any goals set in the session, any interventions used, the date and time of any events, and a detailed record of any observations made during the session.
Write SOAP Notes Immediately Following a Session
It’s strongly recommended that you develop SOAP notes immediately after the speech therapy session. Recalling details is much easier when events are still fresh in your mind. If you wait too long to write up the notes, details may become distorted or forgotten, leading to misunderstandings and inaccurate records.
Make Notes Easy to Understand
Having legible notes ensures that third parties can understand and interpret information. Avoid any kind of shorthand or obscure abbreviations when writing SOAP notes for speech therapy.
Arrange your notes logically and chronologically and separate each section clearly. This improves the readability of your notes and makes it easier for others to understand the information. It’s possible that third parties may need to use your notes for diagnostic purposes or accommodations, so they must be accessible.
Use Direct Quotes
If possible, use direct quotes to illustrate client progress. For example, if the client was able to say a particular word for the first time during their speech therapy session, you could use a direct quote to note this. Doing so provides a more accurate and vivid representation of what occurred during the session. It’s also a useful way of recording client symptoms and progress objectively.
Include Measurable Data
Where possible, include measurable data to give a more accurate report of the client’s progress. For example, if you notice that they’re able to pronounce a certain phrase correctly, note the number of times they could say it in your notes. This provides an objective measure of client progress, which can be used to inform future interventions.
Compare Progress to Previous Sections
Comparing the client’s progress to performance in previous sessions can be illuminating. It allows you to see how they’ve improved over time and any areas that may need additional work or intervention.
By pointing out this information to the client, you can help encourage and motivate them as they strive towards their goals. You can also use this data to adjust the plan of action to better support the client’s needs. It’s a powerful way of demonstrating their progress and provides a sense of accomplishment.
Do a Double-Check
Last, but not least, it’s essential to double-check SOAP notes before submitting them. Some insurance providers may reject reimbursement claims if any sections are missing, so check for gaps or inconsistencies. Even the most experienced clinician can make mistakes (especially when managing a busy caseload), so take the time to review your notes for accuracy and completeness.
Questions to Answer with Your Speech Therapy SOAP Notes
A helpful way of framing your SOAP notes for speech therapy is to ask yourself what information you’d hope to gain by reading someone else’s notes. You can even run through a checklist of questions to ensure you include relevant information.
Here are a few questions to consider when writing SOAP notes:
- What are the client’s goals?
- In what areas is the client progressing?
- In what areas does the client need improvement?
- Is the client ready to finish speech therapy services?
- How was the client’s attitude and behaviour?
- Should any changes be made to their treatment plan?
- What was the outcome of the session?
Asking yourself these questions helps ensure your SOAP notes provide a comprehensive overview of the client’s progress. This also helps to make sure that all relevant information is captured, which can be helpful for third parties that may need to access the notes.
Examples of SOAP Notes for Speech-Language Pathologists
Here are two fictional examples of SOAP notes for speech-language pathologists:
Example 1: Initial Evaluation SOAP Note
Subjective:
- Client presented with concerns about difficulty speaking clearly and being understood by others.
- Client also mentioned feeling self-conscious about their speech and avoiding social situations because of it.
Objective:
- Client demonstrated significant difficulty with articulation and phonological processes, including substitutions, omissions and distortions.
- Client also displayed moderate receptive language delays in understanding complex instructions.
Assessment:
- Based on initial evaluation data, the client is presenting with a severe speech disorder impacting their daily communication skills. Further assessment is needed to determine specific areas of need for treatment.
Plan:
- Refer the client for further assessments, including formal speech and language evaluations.
- Begin therapy sessions to address speech sound disorders, incorporating evidence-based techniques such as motor-based approaches and phonological awareness activities.
- Provide education and resources for family members to support the client’s communication needs at home.
Example 2: Progress Note
Subjective:
- Client reports progress with speech therapy sessions and increased confidence in their verbal communication.
Objective:
- Client demonstrated improved articulation skills, reducing the number of errors from 60% to 20%.
- Client also displayed improved expressive language abilities, using more complex sentence structures.
Assessment:
- Based on progress data, the client is showing significant improvements in both articulation and expressive language skills. Client’s self-esteem and confidence have also improved.
Plan:
- Continue therapy sessions focused on speech sound disorders, incorporating activities to further improve articulation accuracy.
- Expand therapy goals to include increasing expressive language abilities and targeting specific communication situations identified by the client as challenging.
- Encourage continued practice of communication strategies in daily life.
- Provide resources for ongoing support and practice at home.
- Schedule a follow-up assessment in 2 months to monitor progress and adjust therapy goals as needed.
Benefits of Using Electronic Speech Therapy Notes
Using an electronic method of recording SOAP notes for speech therapy provides many benefits for busy clinicians:
- Time-efficient: Typing notes into a computer or tablet is much faster than handwriting each note. This can save significant time and energy during a session, allowing clinicians to spend more time engaging with their clients.
- Accurate and easy to read: Computer-generated text is much easier to read than handwriting, especially if multiple clinicians need to access the notes.
- Searchable: Electronic notes can easily be searched using keywords, saving time when revisiting previous notes or looking for certain topics. This makes it easier to access information quickly and efficiently.
By taking advantage of these features, clinicians can spend more time focusing on client progress and goals, and less time worrying about note-taking. Ultimately, this can help to improve the quality of care that clients receive.
Write SOAP Notes for Speech Therapy with Power Diary
Power Diary is a comprehensive client management and appointment booking solution that will help streamline your practice. Our intuitive user interface makes it easy to capture SOAP notes for speech therapy in an efficient and secure way.
Practice Management Software for SLPs
Practice management software transforms the daily grind for Speech-Language Pathologists into a smoother, more efficient process. The software’s ability to store detailed, accessible SOAP notes allows you to document client progress accurately and securely. This not only helps in tracking therapeutic outcomes but also provides a record for future reference, contributing to a more coordinated care approach. It’s like having a digital assistant that organizes schedules, keeps detailed client notes available when needed, and ensures everyone on the team is on the same page.
If you’re interested in learning more about Power Diary and how it can help you write SOAP notes for speech therapy, start a free trial today.