Writing clinical progress notes is vital to a practitioner’s job and to the running of a successful practice. It helps you keep track of client progress, ensures continuity of care when referring the client to another practitioner for other forms of treatment, and helps you comply with record-keeping guidelines of professional associations or even local government. Notes may also be used in legal proceedings and, as such, it’s critical to consistently and accurately document client progress.
But just because it’s important doesn’t mean that it’s completely straightforward.
Various standard and accepted formats simplify the creation of clinical progress notes. Using a standard format can save your practice (a lot of) time and money, help to ensure your records are comprehensive, and help third parties to understand your notes more easily.
Two commonly used progress note formats are SOAP notes and DAP notes. This article examines how they work, their differences, and which format will work best for your practice.
SOAP Notes
SOAP notes are a widely used standard format for clinical progress notes. In particular, SOAP notes are ideal when monitoring clients diagnosed with multiple conditions, since practitioners specialising in different fields might be involved in the client’s treatment.
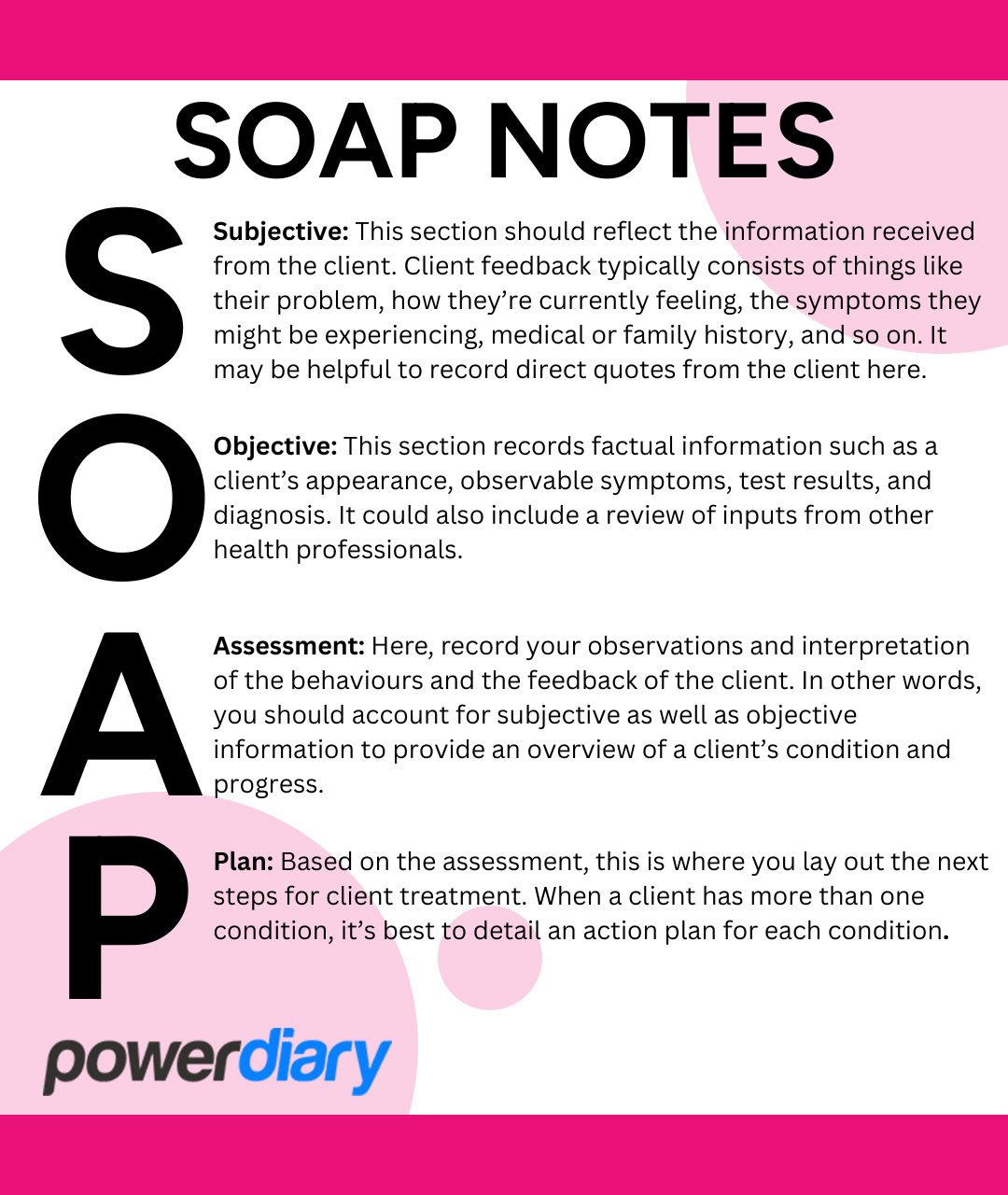
SOAP notes have four sections:
- Subjective: This section should reflect the information received from the client. Client feedback typically consists of things like their problem, how they’re currently feeling, the symptoms they might be experiencing, medical or family history, and so on. It may be helpful to record direct quotes from the client here.
- Objective: This section records factual information such as a client’s appearance, observable symptoms, test results, and diagnosis. It could also include a review of inputs from other health professionals.
- Assessment: Here, record your observations and interpretation of the behaviours and the feedback of the client. In other words, you should account for subjective as well as objective information to provide an overview of a client’s condition and progress.
- Plan: Based on the assessment, this is where you lay out the next steps for client treatment. When a client has more than one condition, it’s best to detail an action plan for each condition.
DAP Notes
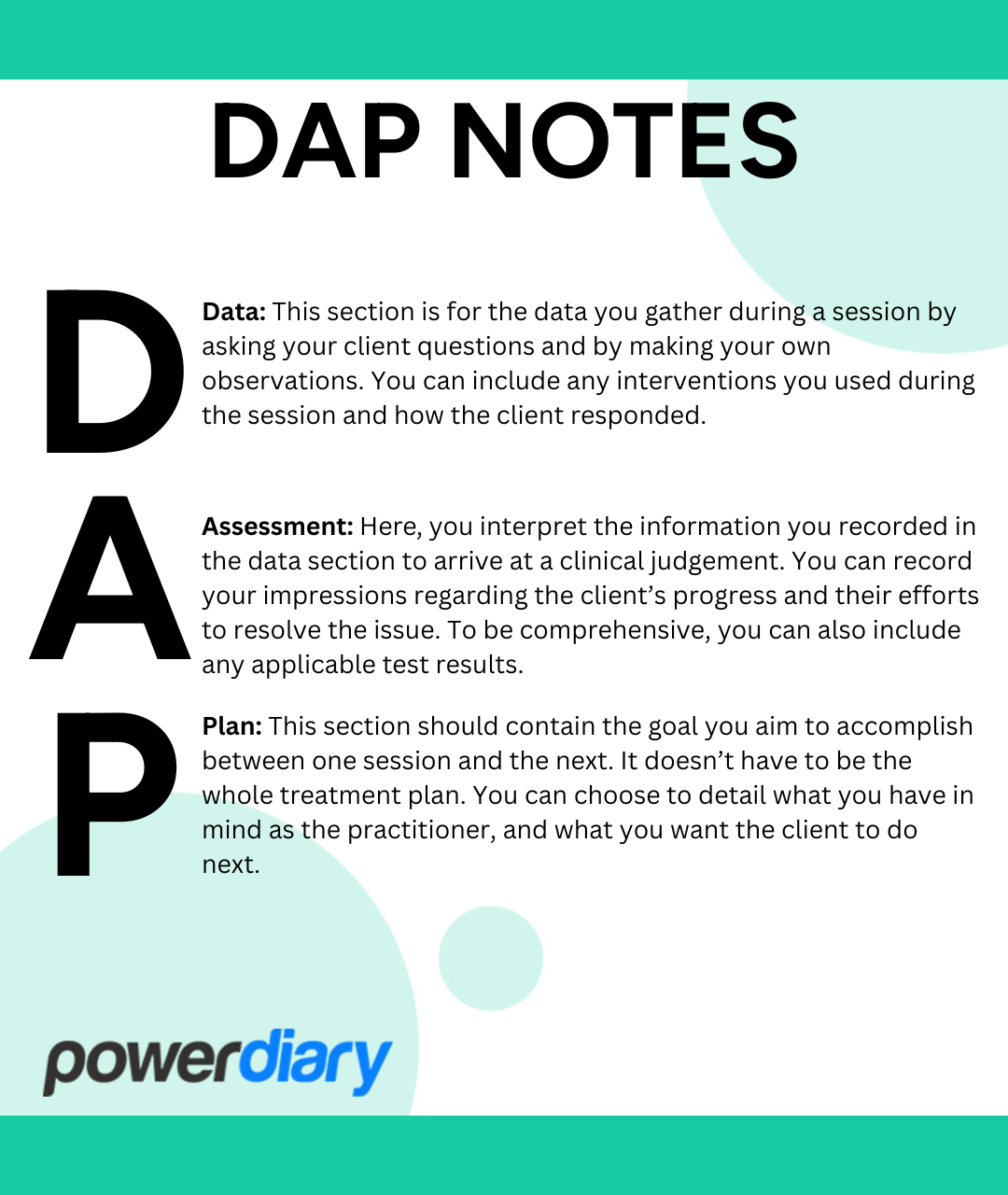
DAP stands for Data, Assessment and Plan, which are the three sections where practitioners record the information provided, clinical observations and a treatment plan.
DAP progress notes are similar to SOAP notes except that the Subjective and Objective sections are combined into one section called Data:
- Data: This section is for the data you gather during a session by asking your client questions and by making your own observations. You can include any interventions you used during the session and how the client responded.
- Assessment: Here, you interpret the information you recorded in the data section to arrive at a clinical judgement. You can record your impressions regarding the client’s progress and their efforts to resolve the issue. To be comprehensive, you can also include any applicable test results.
- Plan: This section should contain the goal you aim to accomplish between one session and the next. It doesn’t have to be the whole treatment plan. You can choose to detail what you have in mind as the practitioner, and what you want the client to do next.
Some practitioners add a section called Response, which changes a DAP note into a DARP note. The Response section is for recording how a client responds to the feedback you give them. Separating this from the Assessment section can be helpful when, for example, a client tends to get defensive, and you feel it’s a primary aspect to account for during treatment.
SOAP Notes vs DAP Notes
Here’s where we tell you what you really want to know: what’s better, SOAP notes or DAP notes?
SOAP notes may be preferred by practitioners who wish to separately record subjective data, such as client symptoms, history or other information the client provides, and objective, measurable data, such as vital signs or test results.
Some practitioners may prefer to use DAP notes as they allow for the combination of both subjective and objective data in the Data section, streamlining the note-taking process by eliminating the need to separate the two types of information into distinct sections.
Ultimately, using SOAP or DAP notes comes down to individual preference.
10 Tips for Writing Good Progress Notes, Whether You’re Team SOAP or Team DAP
Though clinical progress notes should be as comprehensive as possible, they shouldn’t consume very much of your time. Here are some tips to help you be thorough and efficient:
- Review previous notes to refresh your memory on a client’s progress over time.
- Write progress notes as soon as possible after a session, if you don’t do it during the session itself.
- Use quotation marks when recording a client’s direct words.
- Capture the date and time of events as reported by the client.
- Keep your notes as short as possible; don’t include any irrelevant information.
- Write in a professional, simple style so that anyone can understand what you’ve written. Avoid abbreviations.
- As the author, make sure your notes are always signed so that there’s a clear “paper trail”.
- This goes without saying, but if you handwrite your notes, write legibly!
- Use the same procedure every time you make changes or corrections to your notes (such as using a one-line strikethrough to keep original information visible, noting “error” next to it, correcting the information, and initialling the change. This allows the reader to view any changes made)
- To speed up the process significantly, use EHR software and preconfigured note templates.
Write Clinical Notes With Power Diary
If you’re serious about saving yourself time and growing your practice, the best way to do it is to use practice management software like Power Diary.
Power Diary makes it easy to select or create preconfigured note templates with drop-down menus, tick boxes, images, and much more to complete your notes quickly. This helps you to take notes during a session in a way that isn’t disruptive to the client and frees you up to focus on other things once a session is complete. You don’t need to be seated behind a laptop, either; you can use Power Diary with only a cell phone or tablet in hand.
Sign up for a free trial today to see for yourself how Power Diary will revolutionise the operation of your practice!